Adarshini 's E log
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
CASE DISCUSSION:
A 40 yr old male patient came to the hospital with the chief complaints of pain in the right hypochondrium since 5 days.
HISTORY OF PRESENT ILLNESS:
patient was apparently asymptomatic 10 days back .when he had an alcohol binge of 300-500 ml of whisky he complained of diffuse burning sensation in the abdomen, relieved on treatment in private hospital locally followed by :
*right upper quadrant pain since 5 days, which is throbbing in nature, non -radiating, not associated with vomitings, loose stools, stool consistency was normal, no h/o steatorrhoea,melena and belching type of pain, .;aggrevated on inspiration , associated with fever which is of high grade and continous type, associated with chills and no rigors which is persistent for 5 days and subsided 3 days back by taking medication in private hospital , not associated with cough, shortness of breath, no h/o jaundice.
PAST HISTORY:Not a known case of Diabetes mellitus, Hypertension, Asthma, TB, CKD, CVD.
No past surgical history.
PERSONAL HISTORY:His appetite was decreased, takes mixed diet, bowel and bladder movements were regular.
K/c/o chronic alcoholic since 20 yrs. , last binge of alcohol 7 days back. (1/2 bottle whisky). Patient initially started drinking toddy since childhood along with his family almost 250ml and gradually increased to 1 lt/day, Tolerance(+). Started consumption of alcohol(whisky) since 20 yrs, which he took 90 ml initially and then gradually increased to 360ml per day. Eye opener since 4 yrs due to financial crisis .
K/c/ o chronic smoker since 12 years(12-15 bidis per day).
GENERAL EXAMINATION:patient is conscious, coherent, co-operative, well oriented to time, place and person ,moderately built and moderately nourished.
No signs of pallor, icterus, cyanosis, clubbing, kylonechia, pedal edema and lymphadenopathy. In view of chronic alcohol consumption and tobbaco smoking psychiatry referral was done.
On referral to psychiatry I came to know that patient had no palpitations, sweating, tremors during abstinence for 3-4 months every year during new year event.
Smoking since 12 years - (10 cigarretes /day).
No h/o Head injury and seizures
No h/o other substance use,
No h/o hearing of voices,
No h/o suicidal ideas,crying spells,
No h/o grandiose ideas/flight of ideas.
No h/o psychiatry illness in family.
VITALS: pt is Afebrile.
BP:110/60mm hg.
RR:14cpm.
PR:60bpm.
GIT: On examination:
* Abdomen is scaphoid in shape. Umbilicis is central.
* Tenderness (+)in rt. Upper quadrant. Which is increasing on deep inspiration.
* No organomegaly.
* Hernial orifices are free.
* No free fluids and audible bruits.
* Bowel sounds(+).
RESP. SYS: position of trachea is cental.
NVBS- heard on both sides but decreased on right infra scapular area.
BAE: (+).
CNS:level of consciousness: Alert
Speech: Normal
Cranial nerves,Motor and sensory system are Intact.
GCS:15/15.
No signs of meningeal irritation.
CVS:S1 and S2 are heard
No murmurs.
INVESTIGATIONS:CBP,CUE, ECG, CXR, LFT, RFT, USG Abdomen.
*LFT: TOT. BIL:*1.28 mg/dl
DIRECT BIL. : *0.22 mg/dl
SGOT:25 IU/L
SGPT:27IU/L
TOT. PROTEIN:6.6GM/ dl
ALP:*350IU/L
ALBUMIN:2.8 Gm/dl
A/G RATIO : 0.74.
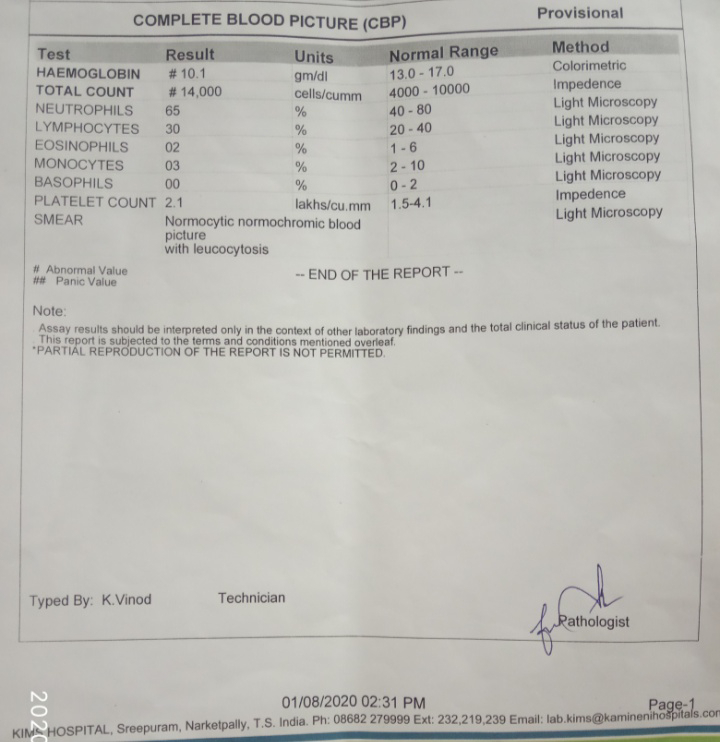
*CBP:
On 1/8/2020
On 3/8/2020
Liver abscess: ?amoebic .
? Bacterial.
With mild rt. Sided pleural effusion and had alcohol dependence syndrome .
TREATMEMENT:
1) INJ. Metrogyl 750mg/IV/tid
2) INJ. Piptaz 4.5 g/iv/tid.
3) INJ. Pantop 40 mg/iv/
4) INJ. Thiamine 100 in 100 ml NS/iv/tid.
5) Tab. Chloroquine 500 /po/od for first 2 days.
|
Tab. Chloroquine 500 mg/po/od. For next 21 days.
6) INJ. Lorazepam 2 mg(if he is anxious and irritable).






Comments
Post a Comment