adarshini e log
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
CASE DISCUSSION:
A 50yr old male Patient from charuvugattu was brought by his attenders(daughter and his brother) to the hospital with complaints of loss of speech since 5 days, right upper limb weakness since 2 days and deviation of mouth to left side since 2 days.
HISTORY OF PRESENT ILLNESS: Patient was apparently asymptomatic 5 days back and then developed loss of speech which was sudden in onset and progressive in nature. No h/o loss of comprehension.
Right upper limb weakness since 2 days which was sudden in onset and progressive in nature. Not associated with tingling and numbness. No h/o weakness in opposite limb.
Deviation of mouth to left side since 2 days which is associated with drooling of saliva fromm right angle of mouth.
h/o loss of nasolabial fold on right side.
h/o difficulty in drinking water.
NO H/O:
*Difficulty in standing from sitting position.
*Difficulty in climbing stairs and wearing chappals.
*Numbness, tingling.
*Nausea, vomiting, diarhhoea
*sensory deficit in feeling clothing.
*Involuntary movements
* wasting/thinning
*Band like sensation
* low back ache
*cotton wool sensation
*postural giddiness, palpitation
* seizures
*Head trauma/ loss of memory
*loss of perception of smell
*Blurring of vision/ double vision
* loss of sensation over face
*Difficulty in chewing food
* Abnormality in taste sensation
* loss of hearing and giddiness.
*Difficulty in swallowing food
* Regurgitation of food.
*Difficulty of shrugging shoulder
* Tongue deviation
*Difficulty in making food bolus
*Tremors/ Tongue fasciculations.
* Fever, vomitings and neck stiffness.
PAST HISTORY:patient had alleged h/o RTA (fall from bike) 7yrs back and had fracture of right medial malleolus for which he underwent open reduction and internal fixation.
not a k/c/o HTN,DM,CVA,CAD,SEIZURES, ASTHMA, TB.
PERSONAL HISTORY:His appetite was normal and takes mixed diet, sleep adequate, bowel and bladder movements were regular. Chronic alcoholic( 90ml per day)and tobacco chewer since 30 yrs .
General examination:pt.is conscious, coherent, co-operative ,oriented ,moderately built and poorly nourished. Comfortable .
Pallor - Negative
Icterus- negative
No cyanosis ,clubbing lymphademopathy,pedal edema.
Skin shows both asymptomatic hypo and hyper pigmented scaly plaques over both upper limbs , trunk and back since 10 yrs. For which dermatology opinion was taken.
VITALS:
Bp: 140/90 mmhg
Pr :80bpm
spo2 :98%at room air
temp :97°F
RR -18cpm
Grbs -136gm/dl
Cvs -s1 s2 heard,no murmurs
Rs -bae +,nvbs heard
P/a soft ,nontender,bowels sound heard,
CNS:
HMF- patient conscious, orientation is not elicited
Speech- motor aphasia(+) .
No h/o delusions, hallucinations.
h/o emotion lability.
cranial nerves: Right left
1 st: smell (+) (+)
2nd :VA/color (+) (+)
Vision
3rd,4th,6th:
pupil size. N N
DLR/CLR. N. N
NO pstosis, nystagmus.
5th :
sensory:over face and buccal mucosa normal
motor :mastication movements - normal.
reflex :corneal andconjuctival -(+)
Jaw jerk (-).
7th:
motor:
Nasolabial (-) (+) more
Fold prominent.
Facial mov. Weakened Normal
sensory: ant. 2/3 rd of tongue -Normal.
secretomotor: moistness of eye and tongue normal,buccal mucosa normal.
8 the nerve:
Rinnes : AC>BC
Weber's:Not deviated to any side I. e,
Central.
No nystagmus.
9and 10 th nerve:
uvula centrally placed and symmetrical,gag and palatal reflex (-).
11 th nerve:
trapezieus : N N
sternocleidomastoid :N N
12 th nerve:
tongue tone normal, no wasting, no fibrillations,no deviation of tongue.
MOTOR SYSTEM
Right. Left
Bulk: Normal. Normal
Tone: u/l. Normal Normal
L/L. Normal Normal
Power:u/l 4/5 5/5
l/l 5/5 5/5
Reflexes.
Superficial reflexes:
Right. Left
Corneal- (+) (+)
Conjunctival- (+) (+)
Abdominal- (-) (-)
Plantar- Decreased Decreased
Deep tendon reflexes :
Right. Left
Biceps. +++ +
Triceps. ++ +
Supinator. +++ +
Knee ++ ++
Ankle. + +
SENSORY SYSTEM:
Not elicited due to motor aphasia.
CEREBELLUM
titubation - absent
Nystagmus- absent
Intensional tremors - absent
Hypotonia-no
Pendular knee jerk
Dysdiadokinesia
MENINGIAL SIGNS
Neck stiffness - negative
Kernigns sign - negative
Brudzinkis sign - negative
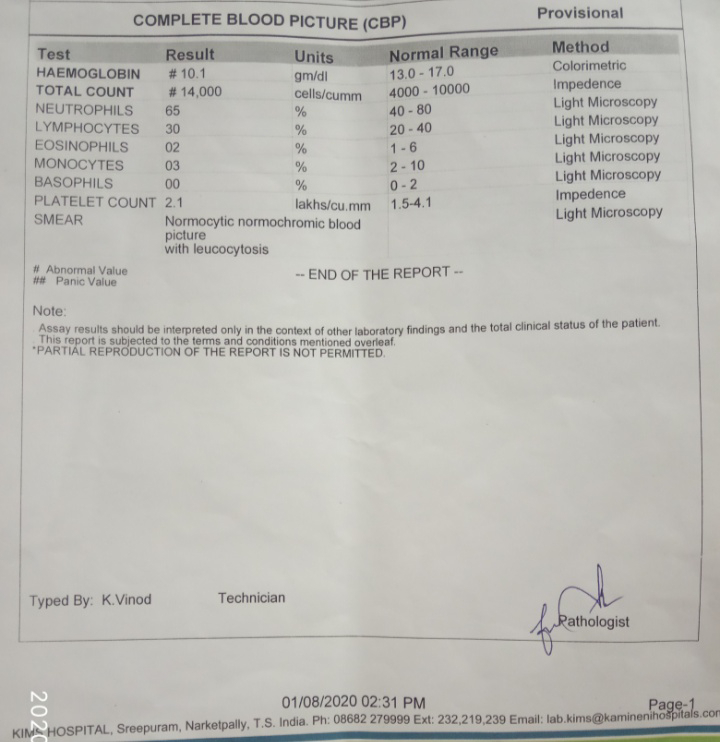
INVESTIGATIONS: on25/7/2020.
*HEMOGRAM :
HB : 15.4 gm/dl.
Platelets : 2.2 lakh/mm3
TLC :7, 400/mm3
RBC: 5.3million/mm3.
*LFT:
TOT.BIL. : 1.21
DI.BIL. : 0.34
SGOT. / AST: 10
SGPT. /ALT : 12
ALK.PH. : 108
Tot. Prot. : 5.4
ALB. : 3.7
A/G RATIO.: 2.29
*RFT
UREA. : 23
CREATININE. : 0.9
URIC ACID : 5.6
CALCIUM.: 10.1
PHOS. : 3.4
SODIUM : 136
K+: 4.1
CL- : 9.7
*RBS: 101 Mg/dl.
*LIPID PROFILE-
Total cholesterol: 177
Triglycerides:180
HDL:95
LDL:108
VLDL:36
*MRI.
DIAGNOSIS: Acute infarct in left frontal lobe with pityriasis versicolor.
TREATMENT
1) TAB. Ecospirin 75mg/od/po
2) TAB. clopidegral 75 mg/od/po
3) TAB. Atorvastatin 40 mg/od
4) TAB. B-PLEX FORTE OD/PO
5) TAB. Benfotiamine 100mg/OD/PO.
6) oint. Ketoconazole L/A.





Comments
Post a Comment