BIWEEKLY INTERNAL ASSESSMENT EXAM
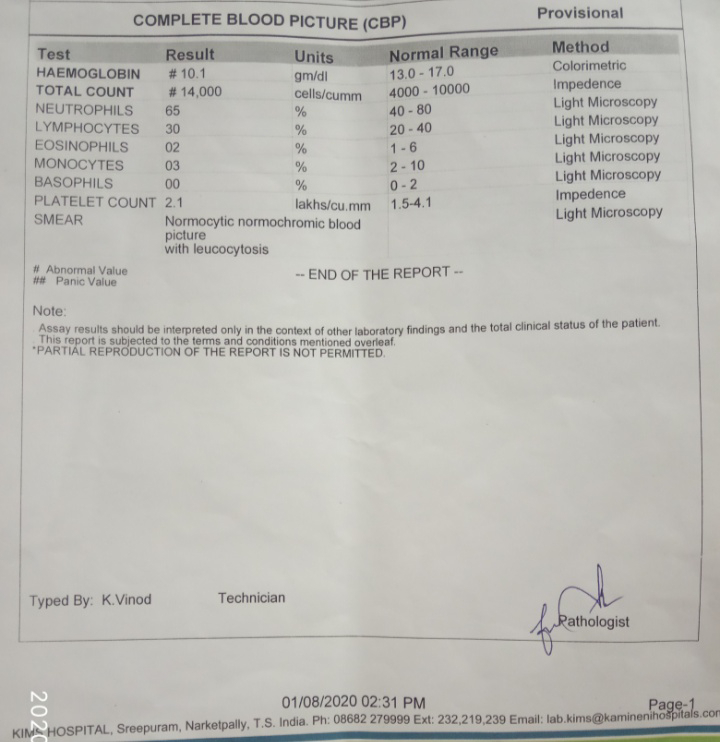
1)Anatomical diagnosis -? Glomerulosclerosis Etiological diagnosis - ?? Nephrotic syndrome secondary to the diabetic nephropathy or CKD. 2)Reasons for I) Azotemia : impaired renal excretion of urea and creatinine secondary to CKD. II) Anemia : decreased erythropoietin. III) Hypoalbunemia: capillary basement membrane and podocytes damage. IV) acidosis: acidification of urine is lost. 3) Rationale : syp potchlor was given because of the hypokalemia.. Inj. NaHCO3 was given because of metabolic acidosis ..Insulin and antihypertensives are given because known case of DM and HTN. Orofer XT was given because of anemia.. Inj. Lasix was given to decrease her volume overload. Spironolactone was given it was a potassium sparing diuretic.Calcium was given to the patient because of hypocalcemia secondary to CKD. Indications of NaHCO3:metabolic acidosis in cardiac arrest, Tricyclic